How does Washington State perform on diabetes care?
Across the country and in our state, a growing population of people are being diagnosed with diabetes, a chronic condition that can be effectively managed and treated with proper screening and intervention.
Figures from the American Diabetes Association (ADA) show that nearly 10% of Washington residents have diabetes, and another 34% have prediabetes – higher than normal blood glucose levels that do not reach the level to be diagnosed as type 2 diabetes. The ADA estimates that nearly 50,000 Washington residents a year are newly diagnosed with diabetes.
As one of the fastest-growing chronic conditions here in Washington and across the country, the cost to provide care nears $10 billion annually in our state. A recent report from the ADA shows that in 2022, the direct cost of diabetes care was $6.68 billion and the indirect care costs were $2.51 billion.
Despite the growing costs of treating people with diabetes, there are clear gaps in care for diagnosed cases. In the primary care setting, our performance on key measures tracking how we evaluate and treat individuals with diabetes can vary greatly by where they live.
“Primary care practices play a crucial role in screening for and treating diabetes. Adhering to consistent and thorough screening and treatment in the primary care setting can make a real difference for the hundreds of thousands of Washington residents with diabetes. Moreover, we need to ensure that all residents have appropriate access to high-quality, affordable care,” said the Alliance Executive Director Drew Oliveira, MD, MHA.
To understand where the care gaps exist, the Washington Health Alliance uses our voluntary All-Payer Claim Database representing more than 4.5 million covered lives in Washington, which tracks seven performance measures related to diabetes.
How our state performs on average across these metrics (rates reported as percentage of covered lives):
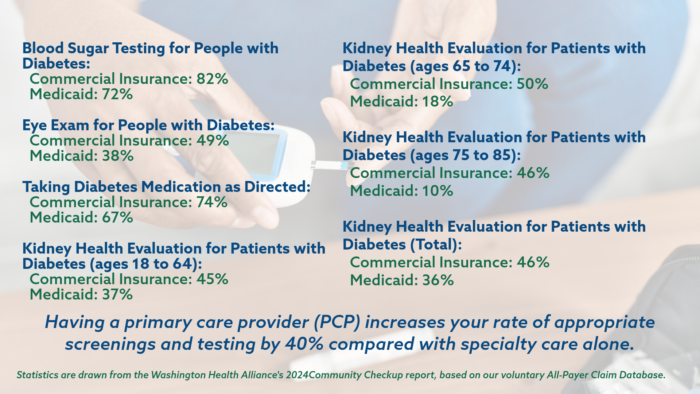
Across these seven measures, as socioeconomic advantage of the insured population decreases, so does the rate for the measure. For example, for commercially insured residents with diabetes, those at most socioeconomic advantage have their kidney health screened at a rate of 41% but those considered least advantaged are screened at a rate of 36%.
This is important because it is well-documented that the prevalence of diabetes increases as income decreases, and this gap is widening.
While these measures reflect the situation for patients with diagnosed diabetes, the Centers for Disease estimates that as many as 1 in 5 people with diabetes do not know they have it. This further highlights the important role primary care providers can play in early screening and intervention.
However, as many as 35% of residents do not have a primary care provider or no annual care and as such are not often receiving routine screenings that could identify the risk of developing diabetes.
What can we do?
Consumer
- Know your risks for developing diabetes.
- Learn all you can about diabetes – ask questions and be sure you are receiving all appropriate screening tests and treatments.
- Connect with a primary care provider to increase the quality of care you receive.
- If you have never had a consultation with a dietician, get one.
- If needed, change your behaviors to improve your health, including diet and exercise.
Employers
- Diabetes care represents roughly a third of your health costs. Review your benefit design annually to ensure your employees and families have access to all aspects of evidence-based care.
- About a third of your population has pre-diabetes with 90% of them not knowing it. Consider direct communications or on-site screening programs to assess metabolic health risks.
- Promote healthy behaviors and lifestyle, which may include onsite healthy cafeterias and safe walking areas.
- Consider plan designs that promote and/or require all members have a primary care provider.
Health Plans
- For fully-insured products, consider plan designs that require all members have a primary care provider.
- Conduct focused outreach to populations at higher risk for developing diabetes.
- For existing members with diabetes, target certain geographies where care gaps are greatest to pull those members into the health system.
- Integrate medical and dental claims to identify care gaps for referral.
- Monitor medication adherence and refer to case management and the member’s PCP when issues identified.
- Work collectively to bring down the price of appropriate medications.
Providers
- If not already done so, have a diabetic registry for your patient populations to be able to track, monitor and assure all patients are accessing appropriate care.
- Identify areas for optimization in the practice to close any omissions of care.
- Consider culture, language and/or race in factoring the care delivery.
- Consider where group visits may be beneficial for a cohort of patients for both care delivery as well as peer-support to maintain treatment adherence.
- Refer patients for dental care regularly to ensure twice annual cleanings to prevent diabetes complications (at each visit).

