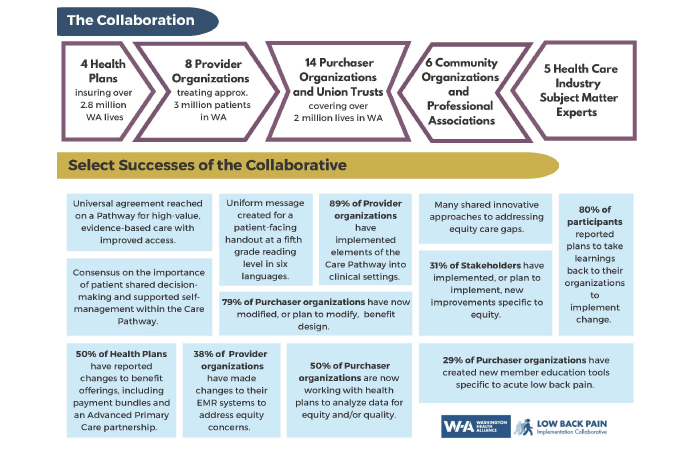
The Low Back Pain Implementation Collaborative brings together more than 30 stakeholders, including health care purchasers, health plan leaders, health care providers, and experts to work on solutions to address the treatment of acute low back pain. It is estimated that 80% of Americans will have some form of back pain in their lifetime, but not all of them will receive high-quality health care to address it.
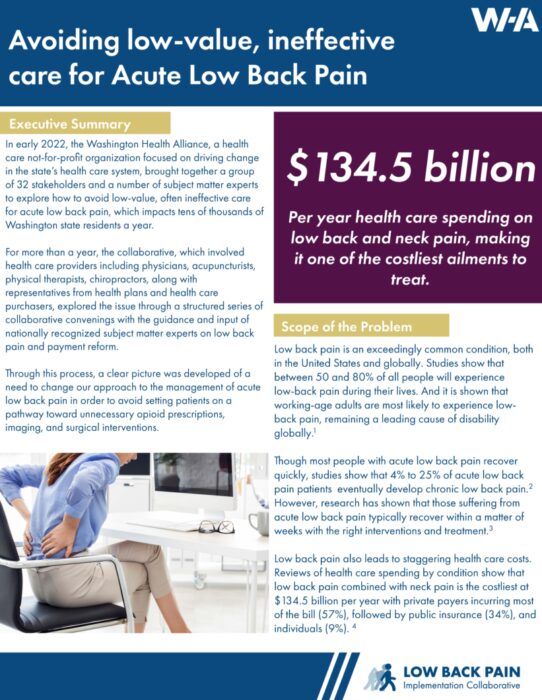
In Washington state alone, the latest data shows that approximately 72,000 people with low back pain received more than 140,000 low-value services at an estimated cost of nearly $10 million in 2020.
A list of collaborative participants and subject matter experts
White Paper
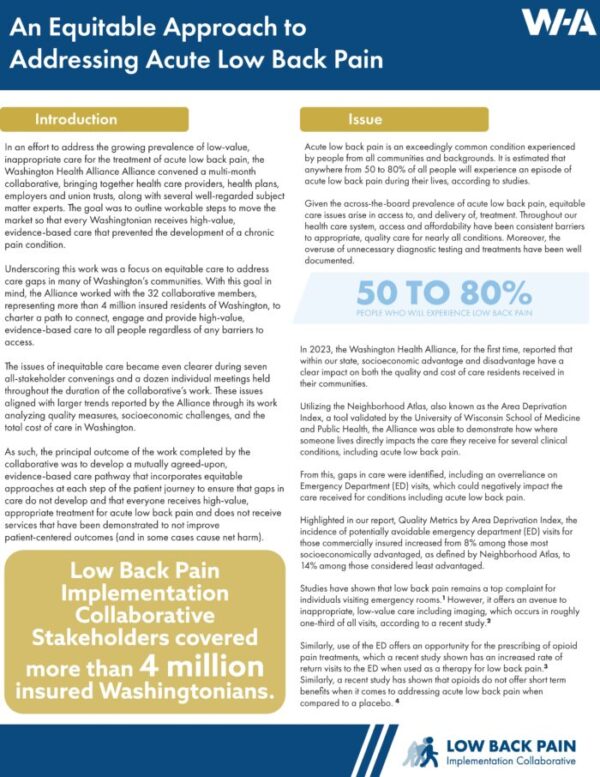
A key focus of the Acute Low Back Pain Implementation Collaborative was to ensure equitable care. Throughout the 18 months of work, the collaborative crafted each step of the care pathway to included efforts to address inequities to ensure care gaps were filled. To have quality in the treatment of acute low back pain, there needs to be equity.
In this paper, the collaborative outlines steps to ensure equity in the screening and treatment of acute low back pain through each of the five steps of the care pathway. We highlight specific efforts each of our stakeholder groups took to ensure access.
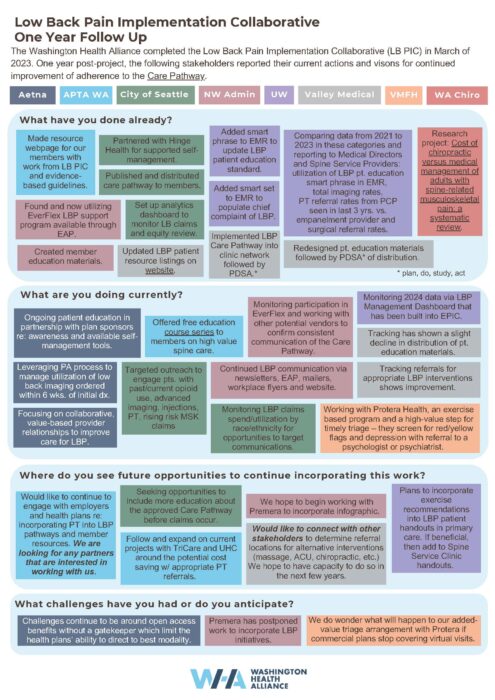
One Year Later
Policy Brief
The brief outlines the broad impact of acute low back pain among the workforce and outlines clear steps that can be taken to ensure that everyone returns to a pain-free life.
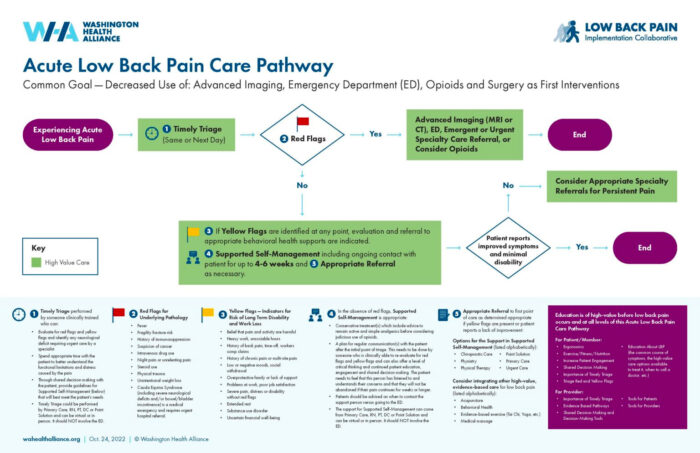
Care Pathway
Acute Low Back Pain Care Pathway |
Collaborative Successes |
|---|---|
 |
|
| Click For Full-Sized Image | Click for Full-sized image |
“While I was initially cautiously optimistic, you pulled off a multi-stakeholder initiative in which people who, at the onset, you’d like to believe had differing incentives and aims, actually came together around meaningful clinical equity and efficiency, that could not only bring about short term significant gains but could also be a template to a much broader approach as we deal with issues of inequity, inefficiency and misallocation of healthcare resources.”
Mark Fendrick, MD
Internal Medicine, University of Michigan
Professor, Department of Internal Medicine and Department of Health Management and Policy, University of Michigan
Director, University of Michigan Center for Value-Based Insurance Design
Resources
As part of its ongoing effort to address the treatment of low back pain, the Washington Health Alliance’s Low Back Pain Implementation Collaborative has collected resources from its stakeholders that highlight efforts to address the issue. The materials below include webinars, patient handouts and member newsletters. The collaborative encourages individuals and organizations share these free materials.
Equity
- Disparities in Spine Care – Dr. David Elton, Optum Labs (video)
- Disparities in Back Pain – International Association for the Study of Pain
- Equity Pause Tool Kit, Virginia Mason Institute
- Inequity Waste Wheel Toolkit, Virginia Mason Institute
Patient
|
“It was really helpful for my team and me to go through this together because we’re engaged in trying to spread some best practices throughout VMFH. This was a platform that really increased the connectivity of our group around our intentions with this. Our Director has since taken and run with some of the initiatives that we had.”
Andrew Friedman, M.D.
Physical Medicine and Rehabilitation
Virginia Mason Franciscan Health
Integrative Care Options
The Alliance’s Low Back Pain Implementation Collaborative, made up of 32 stakeholders, has compiled a list of integrative care options including videos addressing acupuncture, chiropractic care, and physical therapy.
Integrative Care Options:
- Acupuncture for Acute Low Back Pain (video)
- Washington Directory of Licensed Acupuncturists – National Certification Commission for Acupuncture and Oriental Medicine
- Washington Directory of Medical Acupuncturists – American Association of Medical Acupuncture
- Chiropractic Care for Acute Low Back Pain (video)
- Washington Directory of Chiropractors – Washington State Chiropractic Association
- Physical Therapy for Acute Low Back Pain (video)
- Washington Directory of Physical Therapists – American Physical Therapy Association, Washington
“I really valued the variety of people that were present, and it was helpful for everyone to see other angles of the problems and potential solutions. I appreciate your efforts to get big decision-makers all in the room together.”
Morgan Young, D. C.
Associate Medical Director for Chiropractic
State of Washington Department of Labor & Industries
Changing Behaviors
Key to the success of treating acute low back pain is changing the behaviors of the individuals experiencing the condition. Dr. Josh Liao, a board-certified internal medicine physician and the medical director of payment strategy at the University of Washington (UW) Medicine, shares information on changing patient behavior. Liao was among the subject matter experts that assisted the Collaborative.
“The Alliance team addressed a very complex topic and produced an easy to follow product with the Care Pathway.”
Charlene Lind
VP Client Relations
WA Teamsters Welfare Trust
Research
Since the beginning, the Collaborative has reviewed and shared the leading research on acute low back pain treatment, relying on this information to inform materials created through this effort.
Research:
- Low Back Pain Guidelines and Recommendations – The Dr. Robert Bree Collaborative, Foundation for Health Care Quality
- Health Insurance Design and Conservative Therapy for Low Back Pain – American Journal of Managed Care
- Understand Access to Covered Treatment and Services for People with Chronic Pain – Center for Medicare and Medicaid Services
- Active Rehabilitation of Work-Related Low Back Conditions – Washington State Department of Labor and Industries
- Initial Management of Acute and Chronic Low Back Pain: Responses From Brief Interviews with Primary Care Providers – The Journal of Alternative and Complimentary Medicine
- Comparative effectiveness and safety of analgesic medicines for adults with acute non-specific low back pain: systematic review and network meta-analysis
- Landmark Trial: Opioids for Back Pain No Better Than Placebo
Past Updates
Washington Health Alliance Director of Purchaser Strategies Denise Giambalvo and Director of Data Management and Analyst Mark Pregler co-presented “Driving Market Change through Multi-Stakeholder Collaboration” at the Civitas Networks for Health Member Roundtable Meeting on May 23rd.
They reported on the analysis conducted by the Alliance in the first phase of this work, Aligning to Drive Value, with a report for eight employer/purchasers on the amount of low-value that was delivered to their members and families compared to the state average from January 1, 2016 through June 30, 2019 using the Milliman MedInsight Health Waste Calculator™. The highlights include:
• approximately 20% of individuals received at least one-low value service;
• more than $320 million was spent on low-value care by the eight purchasers;
• there was a higher rate of low-value care delivery, approximately 10% more each year, for the purchasers’ populations compared to the state average; and
• one of the most common low-value services provided was the prescription of opiates for low-back pain.
Looking statewide on the issue of low-back pain, analysis using the Alliance’s voluntary All-Payer Claims Database, found that in 2020, more than 72,000 individuals in Washington state received low-value care, including more than 140,000 unnecessary services such as X-rays, MRIs and CT scans and the inappropriate prescribing of opioids, at a combined cost of approximately $10 million.
Since the kickoff of the second phase of this project, bringing together 30 stakeholder organizations to work together “to improve the value of care for all patients with low-back pain in Washington state” in February 2022, there have been convenings both large and small, surveys conducted to share progress across all of the stakeholder groups (health insurance plans, physicians, purchasers, and allies), and the development of a care pathway to support higher quality health care delivery across the state.
If you are interested in joining this exciting project, contact Alliance Director of Purchaser Strategies Denise Giambalvo. The Collaborative is supported by the Arnold Ventures’ Provider Payment Incentives Portfolio.
The Washington Health Alliance’s Low-Back Pain Implementation Collaborative (Collaborative) is continuing to make progress on its mission to “advance the market to improve the value of care for all patients with low-back pain in Washington state.” The Alliance appreciates the commitment of the Collaborative’s 30 participants across all stakeholder groups who are working together to make significant progress on this important initiative:
| Aetna | Proliance Surgeons |
| American Physical Therapy Association | Regence BlueShield |
| Aon | SEIU 775 Health Benefits Group |
| Association of Washington Cities | Seattle Metropolitan Chamber of Commerce/Business Health Trust |
| Bloodworks Northwest | The Boeing Company |
| City of Seattle | UFCW 21 |
| Confluence Health | UW Medicine |
| Davis Wright Tremaine | Virginia Mason Franciscan Health |
| Dr. Robert Bree Collaborative | Washington Acupuncture and Eastern Medicine Association |
| Kaiser Permanente Washington | Washington Health Benefit Exchange |
| King County | Washington Optum Care |
| MultiCare Health System | Washington State Chiropractic Association |
| Point B | Washington State Department of Labor and Industries |
| Port of Seattle | Washington State Health Care Authority |
| Premera Blue Cross | Washington Teamsters Welfare Trust |
In a recent survey, participants reported on the actions they are taking to reduce low-value and increase high-value care for patients with low-back pain.
Health plans reported:
- Setting up telemedicine visits as a first stop for triage
- Directing members to a 24-hour nurse line
- Providing education to members on how to self-manage pain
- Improving an on-line member portal
- Providing more non-surgical care options
- Implementing prior authorizations for advanced imaging and surgery
Health care providers reported:
- Educating primary care providers about care center options
- Instituting baselines to understand the prevalence of low-value care
- Tracking calls to primary care clinics to find out how many result in an Emergency Department or Urgent Care visit
- Referring patients to care options sooner
- Reviewing, updating, and developing patient education materials
- Considering how equity is reflected in care for those with low-back pain
Health care purchasers (employers and union trusts) reported:
- Informing members on the difference between acute and emergent low-back pain
- Considering bundled payment models to allow for more integrated services
- Incentivizing the first point of contact to be with a primary care provider, rather than the Emergency Department
- Promoting health coaching program options to members
- Informing members with a history of chronic low-back pain of free treatment options
- Tailoring benefit design to evidence-based treatment recommendations
Health care allies reported:
- Building awareness of the problem of inconsistent treatment for low-back pain
- Creating purchasing and payment standards that use consistent care quality metrics
- Supporting the use of shared decision making including pain education, self-care, and effective triage
- Working towards producing information videos and investing in educational tools for all stakeholders; health care consumers/patient, providers, purchasers, and plans
During its most recent meeting on April 26th, the group considered various opportunities and recommendations to improve the care delivered to people with low-back pain with the Collaborative’s advisors:
- Dan Cherkin, PhD, Affiliate Professor in Family Medicine, University of Washington; Director of Research, Osher Center for Integrative Medicine; Emeritus Senior Scientific Investigator, KP Washington Health Research Institute;
- Mark Fendrick, MD, Director, Center for Value-Based Insurance Design; Professor, Internal Medicine, School of Medicine and Professor, Health Management and Policy, School of Public Health, University of Michigan, is also a project advisor;
- Andrew Friedman, MD, Section Head of Physician Medicine & Rehabilitation, Virginia Mason Medical Center; Chief of Physiatry, Virginia Mason Franciscan Health; Clinical Assistant Professor, Department of Rehabilitation, University of Washington; and Chair, Industrial Insurance Medical Advisory Committee, Department of Labor; and
- Joshua Liao, MD, MSc, FACP, Associate Professor Medicine; Associate Chair for Health Systems, Department of Medicine; Adjunct Associate Professor, Health Systems and Population Health.
The Collaborative is supported by the Arnold Ventures’ Provider Payment Incentives Portfolio. Contact Alliance Director of Purchaser Strategies Denise Giambalvo for more information on the Collaborative.
Progress on Working Together to Improve Low-Back Pain
As we continue with the Washington Health Alliance’s Low-Back Pain Implementation Collaborative, all of the stakeholders, purchasers, health plans, and health care professionals are identifying ways they can work together to improve the value of health care provided to all of those with low-back pain in Washington state.
As we have learned from our expert advisors, catching low-back pain within the first three months is critical to both alleviate unnecessary doctor visits and improve the likelihood that the patient’s symptoms can be appropriately treated.
Another important foundation to improve low-back care is education, both for providers and patients. Providers are more likely to get the best outcomes when they have the right tools to triage the patient and direct them down the right pathway. Patients also benefit from education because they can learn about care options and ways they can help themselves. In the case of low-back pain, long periods of bed rest can prevent recovery and there is truth to the saying, “motion is lotion.”
We are excited to be working on this important project, supported by Arnold Ventures’ Provider Payment Incentives portfolio, and look forward to sharing more news of our progress.
March 2022
It is estimated that 80% of Americans will have some form of back pain in their lifetime, but not all of them will receive high quality health care to address it. As early as 1985, studies showed the benefits of motion in the healing process and speculation that “help will come in the next decade from a collaborative effort from politicians, industrial leaders and engineers, physicians, psychologists, and biomechanicians.”
Several decades later, that still has not happened. “[B]arriers to optimal evidence-based management include widespread misconceptions of the general public and health professionals about the causes and prognosis of low-back pain and the effectiveness of different treatments, fragmented and outdated models of care, and the widespread use of ineffective and harmful care.”
According to Washington Health Alliance data, approximately 72,000 people with low-back pain received more than 140,000 low-value services an at estimated cost of nearly $10 million in 2020. In addition, a recent review of social determinants of health across 17 countries showed important associations between gender, race, ethnicity, education, occupation and socioeconomic status and low-back pain.
The Alliance’s Low-Back Pain Implementation Collaborative (Collaborative) is working to change that, with the official launch held last month. There are 29 participant organizations representing all stakeholders working together with the mission of “advancing the care for all patients with low-back pain in Washington state.”
A post-launch survey indicated that all participants in the Collaborative felt the orientation with advisors and breakout sessions was relevant to the needs of their organization and several indicated that they are looking forward to developing a plan in which each stakeholder understands their role in reducing medical waste and to supporting equity and reducing health disparities in the treatment of low-back pain.
The Collaborative is supported by the Arnold Ventures’ Provider Payment Incentives Portfolio. For more information on the Collaborative, please contact Alliance Director of Purchaser Strategies Denise Giambalvo.
Low-Back Pain Implementation Collaborative (Low-Back PIC) Launches!
Working to improve the delivery of evidence-based care for low-back pain by all stakeholder groups, the second phase of the Washington Health Alliance’s Driving Value Project, the Low-Back Pain Implementation Collaborative (Collaborative), met as an all-stakeholder group for the first time on February 3rd. Committed to this project are 29 participants, with the majority from purchaser organizations, but also including commercial insurance plans, large provider groups, and several other important organizations, such as the Bree Collaborative, the Washington State Department of Labor and Industries, and the American Physical Therapy Association.
Alliance Executive Director Nancy Giunto said, “We are so appreciative of our partners on this project. It’s an exciting opportunity for us to not only make a significant difference to thousands of people across Washington state but potentially serve as a model for the nation and help millions.” As part of the Collaborative, there will be individual stakeholder meetings to address the unique issues facing health plans, providers, and purchasers. Priorities include:
- benefit design changes to best support employee and members returning to function with optimal health outcomes for purchasers;
- changes to contracts with provider groups to support the use of evidence-based care and patient awareness for plans; and
- identifying evidence-based practices and supporting changes to workflows that support delivery of high-value care for providers.
During the kickoff meeting, the Alliance heard from:
- Andrew Friedman, MD, Section Head of Physician Medicine & Rehabilitation, Virginia Mason Medical Center; Chief of Physiatry, Virginia Mason Franciscan Health; Clinical Assistant Professor, Department of Rehabilitation, University of Washington; and Chair, Industrial Insurance Medical Advisory Committee, Department of Labor.
- Joshua Liao, MD, MSc, FACP, Associate Professor Medicine; Associate Chair for Health Systems, Department of Medicine; Adjunct Associate Professor, Health Systems and Population Health.
- Mark Fendrick, MD, Director, Center for Value-Based Insurance Design; Professor, Internal Medicine, School of Medicine and Professor, Health Management and Policy, School of Public Health, University of Michigan, is also a project advisor.
If you are interested in making a difference in the quality of health care relating to low-back pain across Washington state, contact Alliance Director of Purchaser Strategies Denise Giambalvo.
This project is supported by Arnold Ventures’ Provider Payment Incentives portfolio.
Join the Alliance’s Low-Back Pain Implementation Collaborative (Low-Back PIC)
The Washington Health Alliance is continuing its groundbreaking work to translate its data into actionable health care improvements and invites you to join the effort!
As you may recall, the Driving Value Project, made possible by initial support from Arnold Ventures, leveraged select measures from the Alliance’s reporting on high-value care in the Community Checkup and low-value care in First, Do No Harm to work with purchaser members to improve the value of care received by their 550,000 plan participants. You can download the whitepaper here.
Now, with additional support from Arnold Ventures’ Provider Payment Incentives portfolio, the Alliance is taking those lessons learned and expanding the work to include purchasers, plans, providers, and other health care stakeholders. Over the next year, we will work together to make measurable improvements by implementing patient and provider focused strategies that are underpinned by clinical evidence and aligned incentives.
If you are interested in participating or have questions about the Low-Back PIC, please contact Medical Director, Performance Measurement and Practice Transformation Sharon Eloranta.
Biblography
Amir Qaseem, Timothy J. Wilt, Robert M. McLean, et al; for the Clinical Guidelines Committee of the American College of Physicians . Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med.2017;166:514-530. [Epub 14 February 2017]. doi:10.7326/M16-2367
Cherkin DC. How Can the Intractable Problem of Chronic Musculoskeletal Pain (CMP) Be Effectively Managed? The Need for a Well-Integrated Systems Approach. J Gen Intern Med. 2018 May;33(Suppl 1):4-6. doi: 10.1007/s11606-018-4362-5. PMID: 29633132; PMCID: PMC5902351.
Foster, Nadine & Anema, Johannes & Cherkin, Dan & Chou, Roger & Cohen, Steven & Gross, Douglas & Ferreira, Paulo & Fritz, Julie & Koes, Bart & Peul, Wilco & Turner, Judith & Maher, Chris & Buchbinder, Rachelle & Hartvigsen, Jan & Underwood, Martin & Tulder, Maurits & Cohen, Stephen & Costa, Lucíola & Croft, Peter & Woolf, Anthony. (2018). Prevention and treatment of low back pain: evidence, challenges, and promising directions. The Lancet. 391. 10.1016/S0140-6736(18)30489-6.
Navathe AS, Liao JM. Aligning Value-Based Payments With Health Equity: A Framework for Reforming Payment Reforms. JAMA. 2022;328(10):925–926. doi:10.1001/jama.2022.14606
George, Steven Z.a,*; Goertz, Christinea; Hastings, S. Nicoleb,c; Fritz, Julie M.d. Transforming low back pain care delivery in the United States. PAIN 161(12):p 2667-2673, December 2020. | DOI: 10.1097/j.pain.0000000000001989
O’Connor DA, Glasziou P, Maher CG, et al. Effect of an Individualized Audit and Feedback Intervention on Rates of Musculoskeletal Diagnostic Imaging Requests by Australian General Practitioners: A Randomized Clinical Trial. JAMA. 2022;328(9):850–860. doi:10.1001/jama.2022.14587
Korenstein D, Gillespie EF. Audit and Feedback—Optimizing a Strategy to Reduce Low-Value Care. JAMA. 2022;328(9):833–835. doi:10.1001/jama.2022.14173
Schwartz MR, Cole AM, Keppel GA, Gilles R, Holmes J, Price C. Complementary and Integrative Health Knowledge and Practice in Primary Care Settings: A Survey of Primary Care Providers in the Northwestern United States. Global Advances in Health and Medicine. 2021;10. doi:10.1177/21649561211023377
DHRUVA, S.S., BACHHUBER, M.A., SHETTY, A., GUIDRY, H., GUDUGUNTLA, V. and REDBERG, R.F. (2022), A Policy Approach to Reducing Low-Value Device-Based Procedure Use. Milbank Quarterly., 100: 1006-1027. https://doi.org/10.1111/1468-0009.12595
Ganguli I, Ying W, Shakley T, Colbert JA, Mulligan KL, Friedberg MW. Cascade Services and Spending Following Low-Value Imaging for Uncomplicated Low Back Pain among Commercially Insured Adults. J Gen Intern Med. 2022 Sep 29. doi: 10.1007/s11606-022-07829-2. Epub ahead of print. PMID: 36175757.
Wewege M A, Bagg M K, Jones M D, Ferraro M C, Cashin A G, Rizzo R R et al. Comparative effectiveness and safety of analgesic medicines for adults with acute non-specific low back pain: systematic review and network meta-analysis BMJ 2023; 380 :e072962 doi:10.1136/bmj-2022-072962

Become a member
Get access to the latest news, research, networking events and committees.